Five ways to help care for your child’s atopic eczema
Eczema is a common condition that has a big impact on the lives of children and their families. It can cause soreness, itching and disturbed sleep. Keeping eczema under control takes a lot of effort.
Some parents find it difficult to know how best to look after their child’s skin. They sometimes find seeing their GP unhelpful. Some parents are overwhelmed by the amount of information available and that they don’t know who or what to trust.
In this study a group of parents of children with eczema, and health professionals – nurses, doctors and community pharmacists – have worked together to offer 5 key messages to improve eczema care. Using this knowledge will help.
1) Eczema is more than just dry skin 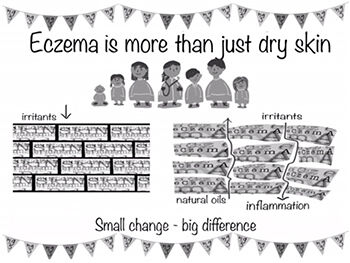
- Children with eczema will always have dry skin
- Dry skin is usually caused by skin inflammation, which makes the skin feel itchy
- Itchy skin leads to scratching, which causes skin damage and then more itching
- Correct eczema treatment can help prevent itching and skin damage
- Moisturisers (emollients) should be used every day, even when the skin is clear
- There is no one cause of eczema (apart from a variety of genes), but lots of individual triggers (such as being tired, teething, cold weather) working together
2) Eczema doesn’t just go away 
- Children with eczema will always have dry skin
- Dry skin is usually caused by skin inflammation, which makes the skin feel itchy
- Itchy skin leads to scratching, which causes skin damage and then more itching
- Correct eczema treatment can help prevent itching and skin damage
- Moisturisers (emollients) should be used every day, even when the skin is clear
- There is no one cause of eczema (apart from a variety of genes), but lots of individual triggers (such as being tired, teething, cold weather) working together
3) Moisturisers are for everyday 
- Moisturisers (emollients) are important for treating and protecting dry skin
- Emollients should be used every day, even when skin is clear to prevent flares
- The best emollient is the one that suits your child and works
- You may need more than one emollient, depending on the dryness of your child's skin, the part of the body affected or time of the year
- Medical moisturisers contain no perfume or detergent
4) Steroid creams are okay when you need them 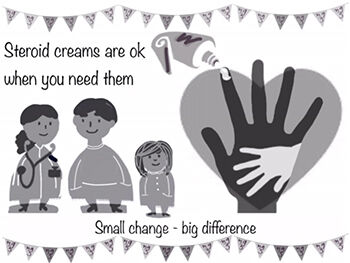
- Steroids creams and ointments (topical steroids) are advised by the NHS as first-line treatments for eczema flares. They are very safe when used as directed
- When using steroid creams, it is important to get control of the eczema. First with a short treatment burst, usually up to two weeks, so that the eczema ‘under the skin’ is treated. Some people with frequent flares find that using topical steroids for two days every weekend on their eczema ‘hot spots’ helps them to then keep control. Talk to your healthcare professional about this
- Steroid creams should be used for short treatment bursts, usually up to two weeks, or as advised by your healthcare professional
- To treat eczema flares effectively, it is common to be prescribed a stronger steroid for 5-7 days and then reduce the strength
- It is important to use enough topical steroid. The finger-tip unit shows the correct amount needed, which is explained in the leaflet in the steroid pack
5) You know your child’s eczema best 
- Your primary healthcare professional, a GP, nurse practitioner or practice nurse can help you to manage your child’s eczema
- Book an appointment just to discuss your child’s eczema, don’t add it on to when you are seeing your health care professional for something else
- Write down how you currently manage your child’s eczema on a daily basis, use this to discuss how treatment can be improved
- Try to keep a diary how your child’s eczema is. Note if their skin is dry or rough skin, itchy, flaking, red, weeping or oozing, bleeding or disturbing their sleep. There is an app to help you do this, https://www.nottingham.ac.uk/research/groups/cebd/resources/poem.aspx
- You can also take pictures of when your child’s eczema is bad, to help your health care professional. It is frustrating when the eczema is better on an appointment day.
- Tell your health care professional how eczema affects your child and your family. You could complete this questionnaire with your child to discuss at the appointment.